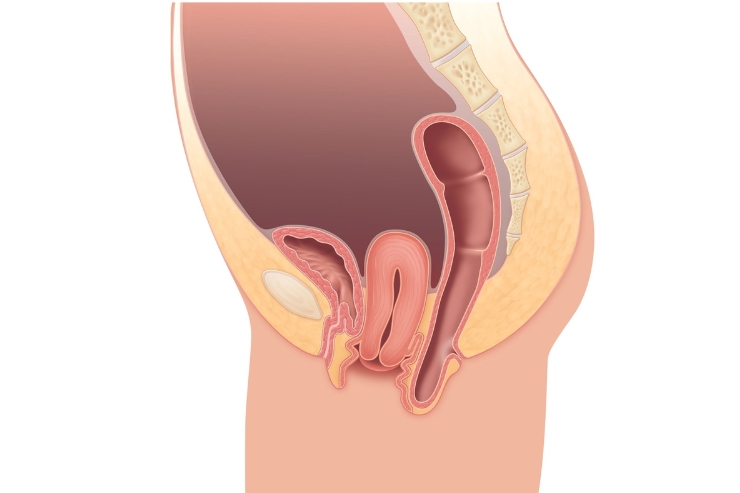
Pelvic Organ Prolapse (POP) occurs when the muscles and tissues that support the pelvic organs—such as the uterus, bladder, rectum, or vagina—become weakened or stretched, causing one or more of these organs to descend into or outside of the vaginal canal. This condition commonly affects women, especially after childbirth, menopause, or pelvic surgery, and its severity can range from mild discomfort to significant interference with daily life. Contributing factors include age, repeated heavy lifting, obesity, chronic coughing, and constipation, all of which can increase pressure on the pelvic floor muscles.
Symptoms of pelvic organ prolapse can vary based on the organs involved and the degree of prolapse. Common complaints include a feeling of pressure or fullness in the pelvis, a visible or palpable bulge in the vagina, urinary incontinence or retention, difficulty with bowel movements, and discomfort during sexual activity. Many women describe a sensation of “something falling out” of the vagina. These symptoms may worsen after prolonged standing, lifting, or physical exertion and often improve when lying down. In some cases, prolapse may be asymptomatic and detected only during a routine pelvic exam.
Management of POP depends on the severity of symptoms and the patient’s health status and preferences. Non-surgical treatments include pelvic floor muscle training (Kegel exercises), lifestyle modifications, and the use of a vaginal pessary—a device inserted into the vagina to support the organs. Surgical options may be considered in more advanced cases or when conservative measures are ineffective. Surgery typically involves repairing the weakened tissue or using mesh to provide added support. Recovery and long-term success depend on the type of repair and adherence to pelvic health practices. With timely diagnosis and proper management, most women with pelvic organ prolapse can regain comfort, confidence, and quality of life.
Services
- Pregnancy
- Menstrual Disorders
- Menopause
- Pelvic Inflammatory Disease
- Endometriosis
- Polycystic Ovary Syndrome
- Cervical Cancer
- Ovarian Cancer
- Uterine Fibroids
- Urinary Incontinence
- Preeclampsia
- Infertility
- Ectopic Pregnancy
- Sexually Transmitted Infections
- Pelvic Organ Prolapse
- Gestational Diabetes
- Abnormal Pap Smears
- Vaginal Infections
- Contraception & Family Planning